One Simple Habit May Reduce Your risk of Dementia
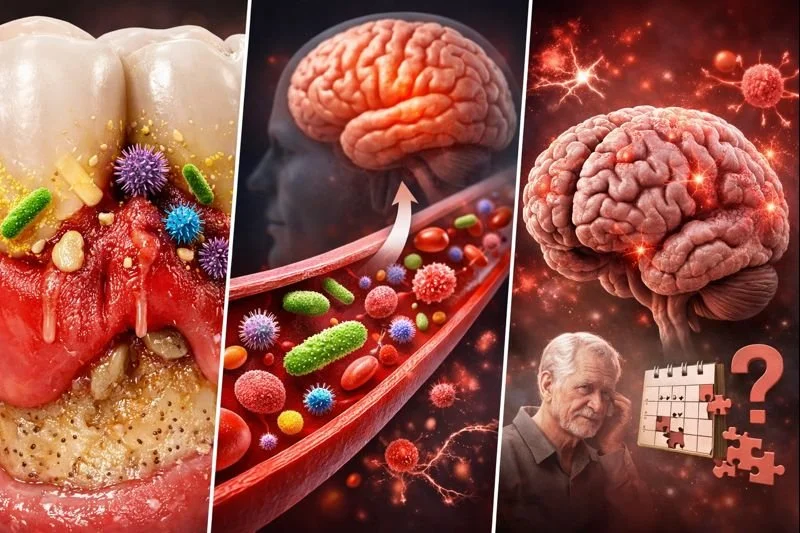
Accumulation of Mouth Bacteria Increases Risk of Dementia
A dental hygiene perspective on flossing, inflammation, and brain health
As a dental hygiene practitioner, I often talk about flossing in the context of cavities and gum disease. However, growing scientific evidence suggests that oral health — particularly the health of the gums — may play a role in long-term systemic conditions, including cognitive decline and dementia.
This conversation is not about fear or blame. It is about understanding how small, consistent habits can reduce biological risk over time.
The link begins with bacteria and inflammation
The mouth contains a complex community of bacteria. When plaque is not adequately removed — especially between teeth, where toothbrushes cannot reach — bacteria accumulate and trigger gum inflammation (gingivitis). If this inflammation becomes chronic, it can progress to periodontal disease.
Multiple systematic reviews show that periodontal disease is associated with elevated systemic inflammatory markers, including C-reactive protein (CRP) and interleukin-6 (IL-6) (Paraskevas et al., 2008; Teeuw et al., 2014). Importantly, randomized controlled trials and meta-analyses demonstrate that periodontal treatment can reduce these markers, supporting the idea that oral inflammation contributes to whole-body inflammation rather than remaining localized to the mouth. (Teeuw et al., 2014)
Why systemic inflammation matters for the brain
Alzheimer’s disease and other dementias are now understood as multifactorial conditions. Chronic inflammation and vascular health are recognized contributors to neurodegeneration.
High-quality systematic reviews and meta-analyses report that individuals with periodontal disease or significant tooth loss have a higher risk of cognitive decline and dementia compared with those who maintain better periodontal health (Leira et al., 2017; Guo et al.,2021; Nadim et al.,2020). While these studies do not establish direct causation, the association is consistent across populations and study designs.
Proposed mechanisms include:
Chronic systemic inflammation affecting the brain
Oral bacteria and inflammatory by-products entering the bloodstream
Vascular changes influencing cerebral blood flow over time
From a preventive health perspective, reducing oral inflammation is a meaningful and achievable target.
Where flossing fits in
Toothbrushing alone does not effectively remove plaque between teeth. Interdental cleaning — including flossing — disrupts bacterial biofilm in areas most susceptible to inflammation.
A major Cochrane systematic review found that interdental cleaning in addition to toothbrushing reduces gingival inflammation compared with brushing alone (Worthington et al., 2019). Reduced gum inflammation translates to a lower bacterial burden and, potentially, a lower inflammatory load on the body over time.
From a clinical standpoint, perfection is not required. Even intermittent flossing is preferable to none.
What dental professionals recommend in Canada
Dental hygienists and dentists in Canada generally recommend:
Daily interdental cleaning, ideally at least once per day
Using floss, interdental brushes, or other tools tailored to individual needs
Prioritizing consistency over perfection
The most important message is simple and evidence-based:
Any flossing is better than no flossing.
A preventive mindset — not a promise
Flossing does not prevent Alzheimer’s disease on its own, and no single habit can eliminate dementia risk. However, reducing chronic inflammation — especially through a low-cost, accessible daily habit — is a practical and meaningful step toward long-term health.
From an evidence-informed dental hygiene perspective, flossing is not just about protecting teeth. It is about supporting the health of the entire body, including the brain.
References